 On our website and social media channels, we have thoroughly explained why and how oral surgery is beneficial. Here’s a reason that has gone unmentioned: it will make you appreciate the solid foods and acidic drinks that you aren’t able to eat or drink immediately after your procedure. Sandwiches, chips, and orange juice should all be avoided after your wisdom tooth removal, dental implant surgery, orthagnathic surgery etc. Too much chewing can possibly re-open the sensitive areas of your mouth, and can cause bleeding or even infection. But don’t worry – we have a few healthy food and beverage recommendations when your mouth is delicate.
On our website and social media channels, we have thoroughly explained why and how oral surgery is beneficial. Here’s a reason that has gone unmentioned: it will make you appreciate the solid foods and acidic drinks that you aren’t able to eat or drink immediately after your procedure. Sandwiches, chips, and orange juice should all be avoided after your wisdom tooth removal, dental implant surgery, orthagnathic surgery etc. Too much chewing can possibly re-open the sensitive areas of your mouth, and can cause bleeding or even infection. But don’t worry – we have a few healthy food and beverage recommendations when your mouth is delicate.
First 24 Hours
For the first 24 hours after your surgery, your teeth/jaw will need some time off. Therefore, smoothies, low-fat jello/puddings, and cold soups will be the most beneficial for your healing process. It is extremely important to refrain from using a straw, as the sucking causes excess strain, which ultimately can delay the healing process. Here are a few recommendations:
Banana Mango Shake- A healthy, filling way to start the day after your surgery. Also, bananas help replace electrolytes and maintain fluid balance within your body.
Applesauce- You can’t eat apples, but this is the next best thing!
Tomato Soup- A great snack even when your mouth isn’t sensitive.
Cold Pasta- Ever tried a Sun-Dried Tomato Basil Orzo? Might be the perfect time to expand your taste buds!
Next Few Weeks
Over the next few weeks, you will start easing into enjoying solid foods again. Here are some tasty transitional foods (some can even help the healing process!)
Broccoli Omelet: Who would’ve thought thathealing from oral surgery could be so healthy? Broccoli contains enough calcium to speed up the healing process, and the eggs provide enough protein to make this a fully substantial meal while taking it easy on your teeth/jaw.
Chicken Salad: Finally some real meat! Chicken that is chopped up into small pieces can be eaten with a salad, or even a cold pasta. The chicken provides the protein, while the salad (with soft vegetables) provides the healthy goodness.



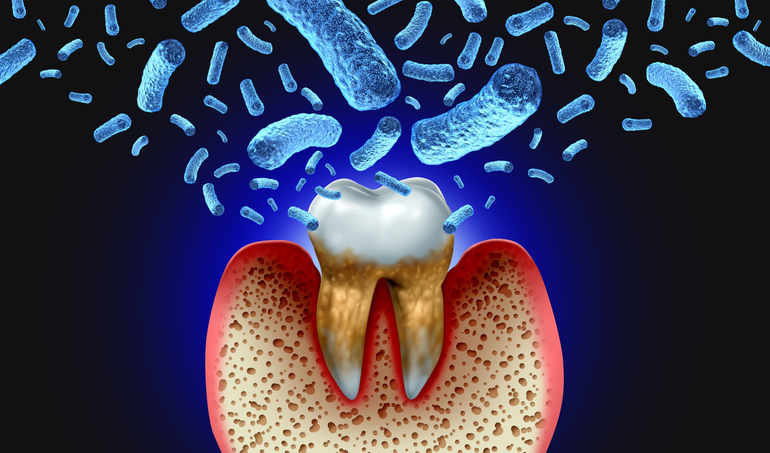 The mouth harbors a diverse and plentiful microbial community due to its hospitable environment. It is warm, nutrient-rich and maintains an ideal pH balance. This highly diverse microflora inhabits the various surfaces of the normal mouth-gums, teeth, tongue, cheeks. What many people don’t realize is that most of the bacteria are beneficial organisms and live in harmony with each other and the human body.
The mouth harbors a diverse and plentiful microbial community due to its hospitable environment. It is warm, nutrient-rich and maintains an ideal pH balance. This highly diverse microflora inhabits the various surfaces of the normal mouth-gums, teeth, tongue, cheeks. What many people don’t realize is that most of the bacteria are beneficial organisms and live in harmony with each other and the human body. A staggering 90% of Americans grapple with periodontal disease annually. This alarming number indicates that most people will, at some juncture in their lives, encounter this dental concern. The depth, intensity, and repercussions of the disease vary among individuals, but it’s clear that oral health is a nationwide concern that cannot be ignored.
A staggering 90% of Americans grapple with periodontal disease annually. This alarming number indicates that most people will, at some juncture in their lives, encounter this dental concern. The depth, intensity, and repercussions of the disease vary among individuals, but it’s clear that oral health is a nationwide concern that cannot be ignored.